Search our Grants
MDA’s research program awards grants to the world’s best scientists investigating promising theories and therapies that may accelerate treatments and cures for families living with muscular dystrophy, ALS and related neuromuscular diseases.
Grant – Winter 2013 – MMD - Darren Monckton, Ph.D.

Darren Monckton, professor of human genetics at the University of Glasgow in Scotland, was awarded an MDA research grant totaling $273,892 over a period of two years to develop new diagnostic tests for myotonic muscular dystrophy type 1 (MMD1, also known as DM1)
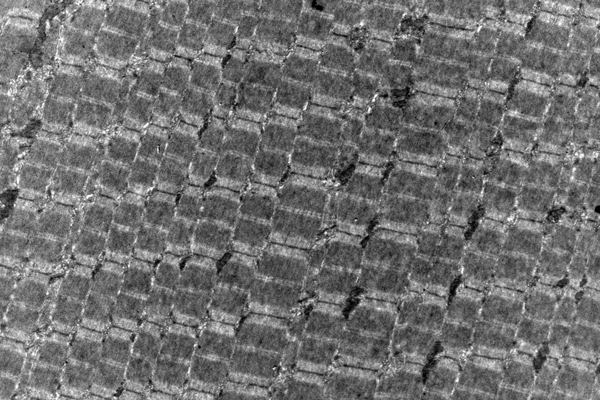
MMD1 is caused by expansion of part of the DNA code in the DMPK gene. Normally, this gene has a small number of repeats of the DNA “letters” CTG. But in people with MMD1, the number of repeated CTG units is 50 or more, and can be over 1000. Furthermore, the number of repeated units in the genes can grow over the lifetime and may differ between different cells.
“In the standard diagnostic test, this genetic instability is ignored,” Monckton says, “and only an average number of repeats is measured.” But the variation may contain important clues to when the disease is likely to begin, and so may provide valuable information to families and individuals with the MMD1 repeat about the future course of disease.
“Using specialized research techniques, we can measure the number of CTG repeats in many cells, then use a computer model to calculate the number of CTGs the patient had at birth,” Monckton notes. “This number much more accurately predicts when symptoms are likely to start. In addition, the CTGs are sometimes interrupted by other groups of three letters, such as CCG, usually leading to milder symptoms,” and later onset in future generations. “Unfortunately, the current genetic test does not take account of age-dependent changes in the number of repeats or detect the presence of these interruptions.”
Monckton will collaborate with genetic testing laboratories to develop new diagnostic tests that will allow the detection of both these important features. In addition to benefits for individual families, the new tests should help make the interpretation of clinical trial results more accurate, since any effects of treatment can be measured against the severity of the genetic mutation.
Funding for this MDA grant began Feb. 1, 2013.
Grantee: MMD - Darren Monckton, Ph.D.
Grant type:
Award total:
Institution:
Country:
Grant - Summer 2012 - DMD/BMD — David Gokhin, Ph.D.
Research associate David Gokhin at the Scripps Research Institute in La Jolla, Calif., was awarded an MDA development grant totaling $180,000 over three years to study the role of a protein called gamma-actin in muscle degeneration and weakness in Duchenne (DMD) and Becker (BMD) muscular dystrophies.
MDA development grants are awarded to exceptional postdoctoral candidates who have the best chance of becoming independent researchers and future leaders of neuromuscular disease research.
Gokhin plans to determine the role gamma-actin plays in regulating the structure, strength and function of the skeletal muscle sarcoplasmic reticulum (SR), a cellular membrane system that houses the calcium that muscles use when they contract. He'll examine how gamma-actin filaments are linked both to the SR and to myofibrils (the force-generating units in muscle contraction).
Next, he'll study SR structure, calcium transport and SR-myofibril connections in the muscles of healthy mice and in those with altered levels of gamma-actin. Lastly, using a DMD mouse research model, Gokhin will examine how elevated levels of gamma-actin affect the DMD disease course.
Gokhin acknowledges progress made in the development of therapeutics for DMD, but says there still is a "gap" in the understanding of basic disease mechanisms.
"In other words, we don't have a convincing answer to the question 'how does a protein defect at the sarcolemma contribute to the cascade of events that leads to muscle wasting,'" he says. "I hope that my research will spark interest in the idea that communication between intracellular and peripheral membranes is an important, yet underappreciated, facet of muscle biology."
Funding for this MDA grant began Aug. 1, 2012.
Grantee: DMD/BMD — David Gokhin, Ph.D.
Grant type: Development Grant
Award total:
Institution:
Country:
Grant - Spring 2014 - Muscle disease - Mariah Baker, Ph.D.

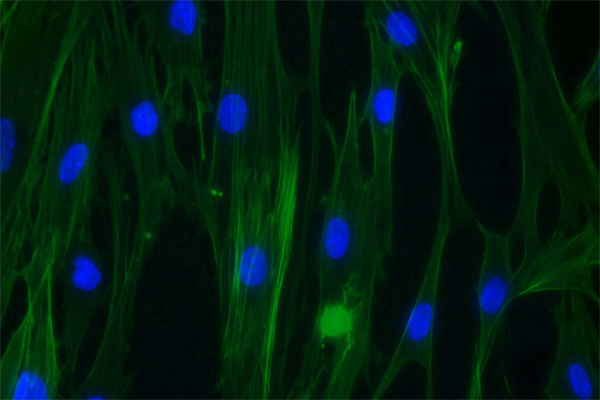
Mariah Baker, a research associate at the University of Texas Health Science Center at Houston, has been awarded an MDA development grant totaling $152,073 over three years to study how the release of calcium molecules is triggered in muscle cells. Improved understanding of this process could have implications for treating a variety of muscle disorders.
Funding for this MDA research grant began May 1, 2014.
Grantee: Muscle disease - Mariah Baker, Ph.D.
Grant type: Development Grant
Award total:
Institution:
Country:
Grant - Winter 2012 - DMD - Kay Davies, M.A., Ph.D.

MDA awarded a research grant totaling $260,000 over a period of two years to Professor Dame Kay Davies, Dr. Lee’s Professor of Anatomy in the department of physiology, anatomy and genetics at the University of Oxford in the United Kingdom. The funds will help support Davies’ development of an effective therapy applicable to all people with Duchenne muscular dystrophy (DMD).
Davies’ approach is to identify a drug that will increase levels in muscle of the structural protein utrophin (similar to dystrophin, the protein deficient in DMD).
“A small molecule drug delivered to the whole body following oral administration can potentially target all affected muscle types, including heart and diaphragm, and would not require [as other therapies under development for DMD do] the use of an immunosuppressant,” Davies explained.
The team will screen candidate compounds for their ability to increase utrophin activity in a mouse model designed to permit real-time quantification of utrophin levels in the living animal.
Davies expects that the new screen will enable her team to rapidly identify new small molecules as lead candidates for DMD.
“Following on the grant from MDA,” Davies said, “we hope to be in a strong position to develop a clinical candidate and, ultimately, to deliver a best-in-class drug for the treatment of DMD.”
Funding for this MDA grant began February 1, 2012.
Grantee: DMD - Kay Davies, M.A., Ph.D.
Grant type: Research Grant
Award total:
Institution:
Country:
Grant - Winter 2012 - DMD - Andrew Ho, Ph.D.

MDA has awarded a development grant totaling $180,000 over a period of three years to Andrew Ho, a postdoctoral fellow at the Institute for Stem Cell Biology and Regenerative Medicine, Stanford School of Medicine in Stanford, Calif. The funds will help support Ho's study of human muscle stem cell regulation and the potential for stem-cell-based therapies in Duchenne muscular dystrophy (DMD). (MDA development grants are awarded to exceptional postdoctoral candidates who have the best chance of becoming independent researchers and future leaders of neuromuscular disease research.)
Currently, there are no effective treatments to reverse the skeletal muscle degeneration associated with DMD. Available therapies treat only the symptoms, not the underlying cause of the disease.
"However, recent progress in a mouse model study suggests that transplantation of mouse muscle stem cells could ameliorate the debilitating effects of skeletal muscle wasting," Ho said.
With colleagues, Ho plans to study human muscle stem cell behavior, with a particular focus on identifying conditions that promote an increase in stem cell numbers. The team also will study the efficacy of a stem cell transplantation approach in a mouse model of DMD to establish whether it can reverse disease-related muscle loss.
Favorable results could point the way toward new therapeutic approaches in DMD.
Funding for this MDA grant began February 1, 2012.
Grantee: DMD - Andrew Ho, Ph.D.
Grant type: Development Grant
Award total:
Institution:
Country:
Grant – Winter 2013 – MG - Socrates Tzartos, Ph.D.
Socrates Tzartos, professor of biochemistry at the Hellenic Pasteur Institute in Athens, Greece, was awarded an MDA research grant totaling $345,033 over a period of three years to develop diagnostic tools for diagnosis of the low-density lipoprotein receptor-related protein 4 (LRP4) form of myasthenia gravis (MG).
MG is an autoimmune disease in which the body’s immune system targets proteins located at the neuromuscular junction, causing weakness. In most patients, the target is the acetylcholine receptor, and in others it is muscle-specific kinase. But 10 percent of MG patients do not have either of these forms, and are said to have seronegative MG (SN-MG). “SN-MG presents a serious gap in MG diagnosis and understanding,” says Tzartos.
Recently, antibodies against LRP4, another protein found at the neuromuscular junction, have been found in some SN-MG patients, and evidence suggests this may be another cause of disease. However, there is not yet a reliable, clinically practical test available for the routine diagnosis of LRP4-MG. Tzartos will be developing such a test by making the protein in animals, purifying it, and comparing a range of assays for their ability to detect the protein. He then plans to test a large number of SN-MG patients to determine the true prevalence of LRP4-MG among this group. Finally, he will explore the pathologic mechanisms at work in LRP4-MG in animal models.
“Since it is known that MG is heterogeneous [varied] in terms of pathophysiology [effects on the body], the outcome of this project is expected to have great impact for this group of MG patients, and provide new insights on the physiology of the neuromuscular junction,” Tzartos says.
Funding for this MDA grant began Feb. 1, 2013.
Grantee: MG - Socrates Tzartos, Ph.D.
Grant type:
Award total:
Institution:
Country:
Grant - Summer 2012 - DMD/BMD — Daniel Michele, Ph.D.

Daniel Michele, associate professor in the department of molecular and integrative physiology at the University of Michigan in Ann Arbor, was awarded an MDA research grant totaling $364,965 over three years to study the underlying mechanisms of muscle weakness and muscle fatigue in Duchenne (DMD) and Becker (BMD) muscular dystrophies. Michele's work could have implications for other dystrophies as well, including limb-girdle muscular dystrophy (LGMD) and congenital muscular dystrophy (CMD).
"Recent work by a number of laboratories has shown that patients and mouse models with DMD show early muscle fatigue, particularly when muscles are active, such as during exercise," Michele explains. "This early fatigue is thought to be primarily due to disruption of the production of nitric oxide in muscle, which helps dilate blood vessels in muscle and increase blood flow during exercise."
Michele notes that there are several forms of the enzymes that produce nitric oxide in muscle, and "it's not exactly clear how nitric oxide production is regulated in muscle during exercise and exactly what causes dysfunction in muscular dystrophy."
With colleagues, Michele is working to determine how nitric oxide production is regulated in muscle and if the normal regulators of nitric oxide production can be targeted to improve muscle blood flow and reduce muscle fatigue during exercise. The team will work primarily with the mdx mouse model (a DMD research model), but also will look at mouse models of other forms of genetic muscular dystrophy and muscle injury.
"Overall, we hope to show that manipulation of the regulators of nitric oxide production will provide potential therapeutic benefit to prevent muscle fatigue," Michele says.
Funding for this MDA grant began Aug. 1, 2012.
Grantee: DMD/BMD — Daniel Michele, Ph.D.
Grant type: Research Grant
Award total:
Institution:
Country:
Grant - Winter 2012 - DD/LGMD - Robert Bloch, Ph.D.

MDA has awarded a research grant totaling $362,295 over a period of three years to Robert Bloch, a professor in the department of physiology at the University of Maryland School of Medicine in Baltimore. The funds will help support Bloch's study of the role of a protein called dysferlin in type 2B limb-girdle muscular dystrophy (LGMD2B) and distal muscular dystrophy (DD, or Miyoshi myopathy).
"Limb-girdle muscular dystrophy 2B and Miyoshi myopathy are caused by mutations in the gene that carries instructions for dysferlin, but the role of dysferlin and its location in muscle cells are controversial," Bloch said.
Bloch and colleagues are working to answer these questions by studying isolated muscle fibers from normal and dysferlin-mutant mice, studying the structure and function of intact muscles from these same mice, and comparing what they observe in mouse muscle to muscles of people with LGMD2B or Miyoshi myopathy.
"The state of research in my area is in considerable flux, largely because of problems that have arisen from attempts to translate studies done in isolated cells to what occurs in muscle tissue in a living animal," Bloch said. "We have been trying to bridge this gap and have been getting results that we did not expect based on earlier work from other laboratories.
"It will take us some time to sort out the differences, but once we do so we anticipate making rapid progress."
Funding for this MDA grant began February 1, 2012.
Grantee: DD/LGMD - Robert Bloch, Ph.D.
Grant type:
Award total:
Institution:
Country:
Grant - Spring 2014 - MMD/DM - Steven Zimmerman, Ph.D.

Steven Zimmerman, a professor of chemistry at the University of Illinois at Urbana-Champaign, has been awarded an MDA research grant totaling $253,800 over three years to develop experimental drugs to treat type 1 myotonic muscular dystrophy (MMD). Conducting experiments in cells and mice with an MMD-like disorder, Zimmerman and colleagues will test a new compound that keeps the MBNL1 protein away from genetic material called RNA. Abnormal interaction between these two substances is believed to play a major role in type 1 MMD.
Funding for this MDA research grant began May 1, 2014.
Grantee: MMD/DM - Steven Zimmerman, Ph.D.
Grant type:
Award total:
Institution:
Country:
Grant – Winter 2013 – MG - Muthusamy Thiruppathi, Ph.D.

Muthusamy Thiruppathi, a postdoctoral research associate in microbiology and immunology in the College of Medicine at the University of Illinois at Chicago, was awarded an MDA development grant totaling $180,000 over a period of three years to pursue ways to restore normal immune system function in myasthenia gravis (MG).
MG occurs when certain cells in the body’s immune system mistakenly target specific proteins on skeletal muscle, causing weakness. The immune system is usually tightly regulated by immune cells called regulatory T cells. In other autoimmune disorders, it is now recognized that there is a defect in the number or function of these cells, and that this contributes to the development of autoimmunity (a condition in which the body's immune system mistakenly attacks its own tissues).
Thiruppathi and colleagues recently have shown that in MG, the number of regulatory T cells is normal, but they do not function properly to suppress unwanted immune responses. “We will now thoroughly examine the nature of this immune defect in MG,” he says, using blood cells collected from individuals with MG and unaffected individuals.
Thiruppathi also will be exploring a strategy to enhance the function of these cells using a natural immune system growth factor called granulocyte-macrophage colony-stimulating factor.
By developing a deeper understanding of exactly how the immune system goes awry, it may be possible to “change the approach to the treatment of myasthenia gravis from global, nonspecific immune modulation to focused, individualized, cellular therapy,” he says.
Funding for this MDA grant began Feb. 1, 2013.
Grantee: MG - Muthusamy Thiruppathi, Ph.D.
Grant type:
Award total:
Institution:
Country:
Grant - Winter 2012 - CMT - Garth Nicholson, M.D., Ph.D.

MDA awarded a research grant totaling $420,000 over three years to professor Garth Nicholson at the ANZAC Research Institute, University of Sydney in New South Wales, Australia.
The funds will help support Nicholson's research into the biological and cellular effects caused by mutations in the copper transport gene ATP7A in Charcot-Marie-Tooth disease (CMT).
Nicholson and colleagues have discovered that mutations in the copper transport gene ATP7A cause slow but progressive degeneration of the long ends (axons) of the nerve cells called motor neurons that send signals to the limb muscles.
The ATP7A protein is essential for human copper metabolism; it is involved with the delivery of copper for physiological processes, and also in maintaining copper balance in humans.
Nicholson's team has shown that mutant ATP7A protein does not traffic copper properly in the presence of elevated copper levels. Now it plans to determine whether ATP7A mutations cause disease symptoms by a mild reduction in intracellular copper movement from motor neurons, or whether the mutations work by some other mechanism such as poor delivery of copper to the distal axon, due to the trafficking defect.
Using human cellular and research mouse models, the investigators plan to determine the biological and cellular effects of the impaired ATP7A trafficking. They will investigate the role of interacting proteins in ATP7A trafficking relevant to axonal copper delivery as a means of exploring the possible mechanistic links between motor neuron disorders and copper; and they will establish a transgenic mouse model that carries mutations in the ATP7A gene.
Funding for this MDA grant began February 1, 2012.
Grantee: CMT - Garth Nicholson, M.D., Ph.D.
Grant type:
Award total:
Institution:
Country:
Grant - Spring 2014 - MMD/DM - Bernard Jasmin, Ph.D.

Bernard Jasmin, a professor in the Department of Cellular & Molecular Medicine at the University of Ottawa, has been awarded an MDA grant totaling $253,800 over three years to examine the role of a protein called staufen 1 in type 1 myotonic muscular dystrophy (MMD or DM) . In this disorder, staufen 1 interacts with abnormally expanded genetic material in muscle cells. Jasmin and colleagues will conduct laboratory experiments to understand the functions of staufen 1, with the goal of developing new strategies for treating type 1 MMD.
Funding for this MDA research grant began May 1, 2014.
Grantee: MMD/DM - Bernard Jasmin, Ph.D.
Grant type: Research Grant
Award total:
Institution:
Country:
Grant – Winter 2013 – MG - David Richman, M.D.

David Richman, professor of neurology at the University of California, Davis, was awarded an MDA research grant totaling $412,500 over a period of three years to study the anti-MuSK myasthenia (AMM) form of myasthenia gravis (MG).
In most people with MG, an autoimmune disease of muscle, individuals make antibodies that react against a part of the muscle called the acetylcholine receptor. But, Richman says, in the AMM form of the disease, antibodies are made against a second protein, muscle-specific kinase (MuSK), also located on the muscle surface. Many of the usual MG treatments are not effective against the AMM form of the disease.
Richman has developed a rat model of AMM, and will use magnetic resonance imaging (MRI) to measure muscle loss in the rats. He also will conduct microscopic and biochemical tests to characterize the affected muscles, and experiments on cells in culture to test various chemical treatments that could have therapeutic potential.
Funding for this MDA grant began Feb. 1, 2013.
Grantee: MG - David Richman, M.D.
Grant type:
Award total:
Institution:
Country:
Grant - Summer 2012 - DMD/BMD — Atsushi Asakura, Ph.D.
Atsushi Asakura, assistant professor at the University of Minnesota Medical School in Minneapolis, was awarded an MDA research grant totaling $378,531 over three years to study how the system of blood vessels known as the vasculature affects muscles in Duchenne (DMD) and Becker (BMD) muscular dystrophies.
Data from recent studies suggests that dystrophin — the protein deficient in DMD — plays a role in blood vessel health and maintenance. The absence of dystrophin in the vasculature results in vascular deficiency, making it likely that disturbed blood flow also is a cause of DMD-related muscle damage.
Therefore, Asakura says, “Definitive treatment of DMD will require both muscle fiber and blood vessel repair.”
With colleagues, Asakura is working to understand how vasculature affects muscle stem cells and regeneration in muscular dystrophies, and to develop a therapy based on growing new blood vessels. The team will examine the effects of increased blood-vessel growth on muscles in a research mouse model of DMD.
“The hope is that at least some, or combinations of, the vascular-targeted therapies will soon have clinical utility and provide current and future human beings living with DMD or other muscular dystrophies enhanced control over their own destiny,” Asakura says.
Funding for this MDA grant began Aug. 1, 2012.
Grantee: DMD/BMD — Atsushi Asakura, Ph.D.
Grant type: Research Grant
Award total:
Institution:
Country:
Grant - Winter 2012 - CMT - Charles Abrams, M.D., Ph.D.
Charles Abrams, an associate professor at SUNY Downstate Medical Center in Brooklyn, N.Y., was awarded an MDA research grant totaling $414,787 over a period of three years to study the role of connexin protein mutations in type 1X Charcot-Marie-Tooth disease (X-linked CMT, or CMT1X).
X-linked CMT differs from other types of CMT in that many people with the disease develop central nervous system signs and symptoms in addition to dysfunction of the peripheral nervous system. (In the CNS long nerve tracts convey information through the spinal cord to the brain, and from the brain down the spinal cord to the peripheral, or outer, nerves and muscles. ThePNS is comprised of nerve fibers outside the spinal cord that send signals to the muscles and relay information from the periphery of the body back to the spinal cord and brain.)
More than 300 mutations in the gene for the connexin 32 protein have been linked to CMT1X. Abrams and colleagues will study whether interactions between mutated connexin 32 protein and a related CNS protein, connexin 47, are the cause of the CNS dysfunction found in the disease.
"We are at the early stages in our understanding of the roles of mutations in connexin 32 in the CMT1X disease process," Abrams said. "We have identified some of the ways in which mutations disrupt the function of connexin 32, but we still do not fully understand why these disruptions lead to both peripheral and central nervous system dysfunction."
Funding for this MDA grant began February 1, 2012.
Grantee: CMT - Charles Abrams, M.D., Ph.D.
Grant type:
Award total:
Institution:
Country:
Grant – Winter 2013 – DD – Laing Distal Myopathy - Leslie Leinwand, Ph.D.

Leslie Leinwand, professor of molecular, cellular and developmental biology at the University of Colorado in Boulder, was awarded an MDA research grant totaling $338,775 over a period of three years to study the causes and treatment of Laing distal myopathy (MPD1).
MPD1 is an inherited muscle disease characterized by early and selective weakness of the lower leg that affects ankle and great toe bending. With time, the disease progresses to other muscles, including those of the neck and face. MPD1 is caused by mutations in a gene called MYH7, which encodes a protein called myosin heavy chain-ß. This protein works in heart and skeletal muscle to create the pulling force that allows muscles to contract, Leinwand says, “but how these mutations lead to disease is unknown.”
Her goal is to learn more about how mutations in MYH7 cause the cellular defects that are at the root of MPD1. Specifically, she is interested in determining the effects of mutations on the ability of multiple myosin proteins to link together, which they must do to function properly. She thinks it’s likely that a defect in that linking ability may reduce the stability of sarcomeres, the basic unit of muscle that exerts the pulling force.
She also will create a mouse model of MPD1 in order to better study the effects of mutation and to test potential therapies. “We hope that our experiments will expose the pathogenesis of the disease and will lead to a successful molecular treatment for MPD1, for which there is currently no treatment,” says Leinwand.
Funding for this MDA grant began Feb. 1, 2013.
Grantee: DD – Laing Distal Myopathy - Leslie Leinwand, Ph.D.
Grant type:
Award total:
Institution:
Country:
Grant - Spring 2014 - MMD/DM - Andrew Berglund, Ph.D.

Andrew Berglund, a professor of biochemistry, biophysics and molecular biology at the University of Oregon in Eugene, has been awarded an MDA research grant totaling $253,800 over three years to pursue changing the shape of the abnormal genetic material underlying type 1 and type 2 myotonic muscular dystrophy (MMD or DM). Berglund and colleagues will conduct laboratory experiments to see whether changing the shape of abnormally expanded genetic material (RNA) in these two forms of MMD can reduce or eliminate their harmful effects.
Funding for this MDA research grant began May 1, 2014.
Grantee: MMD/DM - Andrew Berglund, Ph.D.
Grant type: Research Grant
Award total:
Institution:
Country:
Grant - Winter 2012 - CMD/LGMD - Jeffrey Miller, Ph.D.

MDA awarded a research grant totaling $343,860 over a period of three years to Jeffrey Boone Miller, senior scientist at Boston Biomedical Research Institute in Watertown, Mass., and associate professor of neurology at Harvard Medical School in Boston. The funds will help support Miller’s study of the underlying causes of, and potential therapeutic strategies for, three muscular dystrophies: type 1A congenital muscular dystrophy (MDC1A/CMD), and types 2C and 2D limb-girdle muscular dystrophy (LGMD2C, LGMD2D).
During normal skeletal muscle development, immature muscle cells calledmyoblasts fuse together to form large, tube-shaped cells called myotubes. Myotubes ultimately mature into muscle fibers.
“We find that myotubes formed in culture from human MDC1A, LGMD2C and LGMD2D patient myoblasts, but not normal myoblasts, spontaneously undergo cell death,” Miller said.
Miller and colleagues have found that the abnormal activation of the cell death, caused by the Bax protein and its binding partner Ku70, may underlie the cell-death changes in each of the three diseases under investigation.
In his new work, Miller plans to examine the role dysregulation of the Ku70/Bax pathway plays in muscle development. He first plans to determine whether the abnormal function of proteins that modify Ku70 function cause abnormalities in muscle. In a second set of experiments, he will test the hypothesis that restoring Ku70 function to a normal level will inhibit cell death and decrease the abnormalities in human myogenic cells.
“From our results, we hope to identify potential therapeutic strategies that could be effective for multiple diseases.”
Funding for this MDA grant began February 1, 2012.
Grantee: CMD/LGMD - Jeffrey Miller, Ph.D.
Grant type:
Award total:
Institution:
Country:
Grant - Winter 2012 - CMD - Mahasweta Girgenrath, Ph.D.
MDA awarded a research grant totaling $357,465 over a period of three years to Mahasweta Girgenrath, an assistant professor in the Health Sciences Department at Boston University in Boston. The funds will help support Girgenrath’s work to find a combination therapy to treat type 1A congenital muscular dystrophy (MDC1A).
Girgenrath and colleagues plan to explore strategies designed to inhibit the inflammation and fibrosis (muscle scarring) associated with MDC1A, either alone or in combination with improved muscle regeneration.
The team will conduct their studies in the DyW mouse model, which develops a muscular dystrophy that closely matches the disease process seen in humans with MDC1A.
“We previously have shown that improving regeneration by increased activity of a growth factor called IGF1 improves muscle mass, but does not affect inflammation,” Girgenrath said. The group will now try a therapy designed to prevent inflammation in the muscles of the DyW mice, both alone and in combination with IGF1-based regeneration therapy.
“If successful,” Girgenrath said, “our results may lead to a combination therapy to fight the devastating prognosis of MDC1A.”
Funding for this MDA grant began February 1, 2012.
Grantee: CMD - Mahasweta Girgenrath, Ph.D.
Grant type:
Award total:
Institution:
Country:
Grant - Summer 2012 - DMD/BMD — Adam Engler, Ph.D.

Adam Engler, assistant professor at the University of California, San Diego, in La Jolla, was awarded an MDA research grant totaling $390,000 over three years to study cell-based therapies designed for Duchenne (DMD) and Becker (BMD) muscular dystrophies and other muscle diseases.
Engler and colleagues are working with adipose-derived stem cells, orASCs (stem cells derived from fat). These cells, Engler says, are readily available, can develop into muscle, and — once they become muscle — can integrate into damaged skeletal muscle tissue. But the ASCs so far have been unable to repair DMD-related damage and restore muscle function.
Now Engler’s team, which has demonstrated the function of ASC-derived muscle in the lab, plans to translate those findings into animal models of muscular dystrophy.
The investigators are using a new method to coax ASCs into turning into mature muscle cells that they say should “better mimic” the conditions in which muscle cells in the body mature. This should make the cells more likely not only to integrate into damaged muscle tissue, but also help repair it.
”Stem-cell-based regenerative applications for muscle diseases, including muscular dystrophy, are showing increasing signs of feasibility in our lab," Engler says. "But our research and others' address critical stumbling blocks that currently prevent successful translation of these therapies in animal models of the disease and in humans."
Funding for this MDA grant began Aug. 1, 2012.
Grantee: DMD/BMD — Adam Engler, Ph.D.
Grant type: Research Grant
Award total:
Institution:
Country:
Grant - Winter 2012 - Cell Therapy - Ilona Skerjanc, Ph.D.
MDA awarded a research grant totaling $280,487 over a period of two years to Ilona Skerjanc, a professor in the department of biochemistry, microbiology & immunology at the University of Ottawa in Ontario, Canada.
The funds will help support Skerjanc’s investigation into using cell therapies to enhance muscle repair in any of a number of muscle diseases, including congenital muscular dystrophy (CMD); Duchenne (DMD) and Becker (BMD) muscular dystrophies; and Emery-Dreifuss muscular dystrophy (EDMD).
Several cell sources, including satellite cells (a type of immature muscle cell) and mesenchymal stem cells (derived from bone marrow), are currently under study for potential use in therapies to reverse muscle degeneration and strengthen existing muscle. However, Skerjanc noted, difficulties with these approaches include the requirement for invasive procedures, the availability of suitable donors and a limited potential for long-term benefit.
Skerjanc and colleagues recently showed that human embryonic stem (hES) cells can mature into skeletal muscle via progenitor and myoblast (both immature muscle cell types) stages.
In her new work, Skerjanc will isolate skeletal muscle progenitors from hES cells and examine their ability to engraft into skeletal muscle in a mouse model of DMD.
“The overall goal is to provide a method of hES cell differentiation(maturation) and enrichment that will generate human myoblasts and progenitors for long-term engraftment and future therapeutic applications,” Skerjanc said.
Funding for this MDA grant began February 1, 2012.
Grantee: Cell Therapy - Ilona Skerjanc, Ph.D.
Grant type:
Award total:
Institution:
Country:
Grant - Summer 2012 - DMD — Tathagata Chaudhuri, Ph.D.
Postdoctoral research fellow Tathagata Chaudhuri, at the Perelman School of Medicine at the University of Pennsylvania in Philadelphia, was awarded an MDA development grant (DG) totaling $180,000 over three years to develop a stem cell therapy for muscular dystrophies, including Duchenne muscular dystrophy (DMD), that will lead to muscle regeneration.
MDA development grants are awarded to exceptional postdoctoral candidates who have the best chance of becoming independent researchers and future leaders of neuromuscular disease research.
Some experimental cell therapies for muscular dystrophies are designed to use cells from healthy human donors, but the successful transplantation of cells from one person to another requires the use of immunosuppressants in order to keep the body from rejecting the new cells.
Chaudhuri and colleagues are working on the development of a cell-based therapy that uses a person's own stem cells — adult mesenchymal stem cells (MSCs), which are taken from bone marrow and coaxed into becoming muscle cells.
The team first plans to demonstrate that MSCs can reliably be differentiated(grown) into muscle cells. They'll then use the cells they produce to study muscle regeneration in animal models of muscular dystrophy.
Next, Chaudhuri and his team will determine the optimum time for transplanting the maturing cells into a recipient. They'll monitor the development of the human MSCs in animal models to determine how well the MSCs integrate with existing muscle fibers and whether they have any effect on muscle repair and regeneration over time.
Treatment with adult stem cells that develop into muscle cells may provide a means to correct skeletal muscle function in muscular dystrophy, Chaudhuri says, noting that this type of therapy for DMD and other dystrophies "is currently becoming an increasingly attractive area of research in the muscular dystrophy community."
Funding for this MDA grant began Aug. 1, 2012.
Grantee: DMD — Tathagata Chaudhuri, Ph.D.
Grant type: Development Grant
Award total:
Institution:
Country:
Grant – Winter 2013 – LGMD - Noah Weisleder, Ph.D.

Noah Weisleder, associate professor of physiology and cell biology at Ohio State University in Columbus, was awarded an MDA research grant totaling $405,000 over a period of three years to study muscle repair for development of treatment for limb-girdle muscular dystrophies (LGMD).
In all muscular dystrophies, muscles are damaged during normal use. Part of that damage occurs when the outer membrane of the muscle cell tears under the force of normal muscle contraction. The cell has mechanisms to repair torn membranes, allowing the survival of these damaged cells, but these mechanisms are insufficient in LGMD and other muscular dystrophies.
“These findings suggest that a therapeutic approach that increases membrane repair capacity could have broad efficacy across a number of different muscular dystrophies in human patients,” Weisleder says.
His group has previously shown the importance of a protein called Mitsugumin 53 (MG53) in the repair process, and has demonstrated that it can be directly applied to cells and tissues to increase the repair capacity, including in a rodent model of Duchenne muscular dystrophy (DMD). He will now test this strategy in various rodent models of LGMD, to determine if this protein could be used as a therapeutic approach in humans.
“If MG53 can improve pathology in a number of different muscular dystrophies,” Weisleder says, “it is more likely that this protein therapy could be effectively moved towards clinical trials, as it would be able to treat a relatively large patient population spread across various types of muscular dystrophy.”
While such therapy would not be a definitive cure for any of the muscular dystrophies, it could provide meaningful therapy for patients until definitive treatments for the underlying causes of these diseases are available.
Funding for this MDA grant began Feb. 1, 2013.
Grantee: LGMD - Noah Weisleder, Ph.D.
Grant type:
Award total:
Institution:
Country:
Grant - Summer 2012 - CMT/FA — Jeffrey Milbrandt, M.D., Ph.D.

MDA awarded a research grant totaling $357,366 over three years to Jeffrey Milbrandt, professor and head of the department of genetics, and professor of pathology & immunology, medicine and neurology at Washington University School of Medicine in St. Louis.
The funds will help support Milbrandt's work in determining how Schwann cells contribute to nerve damage (neuropathy) in neuromuscular diseases such as Charcot-Marie-Tooth disease (CMT) and Friedreich's ataxia (FA).
Neuropathies and neuromuscular diseases like CMT and FA are associated with poor function of mitochondria, the energy producer in cells.
In previous work, Milbrandt and colleagues found that mice with mitochondrial deficits in Schwann cells develop a progressive neuropathy. (Schwann cells are a type of support — or glial — cell in the nervous system outside the brain and spinal cord; they support the function and maintenance of nerve fibers, or axons.)
Milbrandt's new project focuses on determining how Schwann cells obtain their energy when their mitochondria are damaged, and the mechanisms by which Schwann cell metabolism causes damage to the peripheral nerves (bundles of nerve fibers that run between the spinal cord and the muscles). He also plans to test whether pharmacological interventions to manipulate Schwann cell metabolism will help restore normal peripheral nerve function.
"For these studies, we will use a mouse model in which mitochondria are dysfunctional specifically and exclusively in Schwann cells," Milbrandt explains. "These mice, called Tfam-SCKO mice, are a good model for these studies because they develop many critical features of human neuromuscular disease and peripheral neuropathy."
Millbrandt notes: "Peripheral neuropathy research is entering a new era as we learn more about how axons are dismantled and the role of glia in maintaining axon health. There are unparalleled opportunities now to develop new treatments for this debilitating condition that is reaching epidemic proportions worldwide."
Funding for this MDA grant began Aug. 1, 2012.
Grantee: CMT/FA — Jeffrey Milbrandt, M.D., Ph.D.
Grant type:
Award total:
Institution:
Country:
Grant – Winter 2013 – FSHD - Rabi Tawil, M.D.

Rabi Tawil, professor of neurology at the University of Rochester Medical Center in Rochester, N.Y., was awarded a one-year MDA research grant totaling $92,222 to develop a biomarker for facioscapulohumeral muscular dystrophy (FSHD).
FSHD is caused by aberrant expression (activity) of a gene called DUX4, which is usually silenced in adult muscle tissue. DUX4 turns on other genes, and activity of these genes is believed to cause disease by multiple mechanisms, including direct toxicity, interference with normal cell function and provoking the immune system.
“Having identified potential therapeutic targets in FSHD,” says Tawil, “it becomes crucial to identify sensitive, disease-related biological markers [biomarkers] that can be easily measured in blood or muscle tissue to assess the effectiveness of future disease-modifying drugs.” FSHD researchers recently came to consensus that development of biomarkers was a top priority for progress in the disease.
Tawil will be investigating whether a small group of these abnormally expressed genes may serve as biomarkers. He will examine muscle biopsies and blood serum from individuals with FSHD and unaffected individuals, and compare the level of proteins made from these genes. Any differences will then be correlated with the overall disease severity and the severity of changes in the muscle.
“At the end of this study we hope to have promising biomarkers for future clinical trials,” he says. “Research is now focused on treatment of FSHD, and consequently having all the tools ready for future clinical trials is essential.”
Funding for this MDA grant began Feb. 1, 2013.
Grantee: FSHD - Rabi Tawil, M.D.
Grant type:
Award total:
Institution:
Country:
MDA Resource Center: We’re Here For You
Our trained specialists are here to provide one-on-one support for every part of your journey. Send a message below or call us at 1-833-ASK-MDA1 (1-833-275-6321). If you live outside the U.S., we may be able to connect you to muscular dystrophy groups in your area, but MDA programs are only available in the U.S.