
In Focus: Straightening the Growing Spine

In the past, children with rapidly progressive neuromuscular scoliosis often underwent growth-stopping spinal fusion. Today, there are more options.
Payton Mueller's parents knew something was amiss by the time he was 9 months old.
 “Payton crawled really early,” recalls his mother, Rachele Krebsbach of Crosby, N.D. “He pulled himself up on furniture at 7-and-a-half months, and he was into everything a lot sooner than I had expected him to be. But then he just kind of stopped doing everything.”
“Payton crawled really early,” recalls his mother, Rachele Krebsbach of Crosby, N.D. “He pulled himself up on furniture at 7-and-a-half months, and he was into everything a lot sooner than I had expected him to be. But then he just kind of stopped doing everything.”
Around the time of Payton’s first birthday in September 2001, Rachele was told he had spinal muscular atrophy (SMA), a genetic disorder in which the motor neurons in the spinal cord are lost, causing profound weakness of the voluntary muscles.
For a long time, Payton could sit up by himself, but it soon became apparent that his spine was curved. “You could look at his back and see that there was a definite curve,” Rachele says. “The bigger the curve got, the less he was able to sit unaided.”
Payton got his first back brace at age 4 and wore one until he was 9, after which he began surgical correction of his spinal curvature. Not long ago, that surgery would have been his first and last, and his spine would have stopped growing at age 9.
But Rachele opted for a relatively new procedure called growing rods, in which adjustable-length rods are inserted into the spine and lengthened approximately every year as the child grows. By the time he turned 12 in September 2012, Payton had undergone three rod-lengthening procedures.
“I wanted to make sure that his body continued to grow,” says Rachele.
Straightening the growing spine
Side-to-side curvature of the spine — known as scoliosis — is a common feature of many neuromuscular disorders. A forward bend to the spine — kyphosis — also can occur, but it isn’t as common.
In Duchenne muscular dystrophy (DMD), a genetic muscle disease with onset of noticeable weakness starting in the toddler years, scoliosis and occasionally kyphosis are common, but they usually don’t become serious enough to require treatment until a child has reached his teens and is nearly full grown.
An operation known as spinal fusion, which straightens the spine but prevents further spinal growth, is commonly done in DMD in the teen years, at a time when relatively little additional growth of the spine would be expected to occur. (See Scoliosis Surgery: Before and After, Quest, August 2002.)
However, straightening the spine in disorders where weakness of the back muscles often causes marked scoliosis long before adult height is reached poses additional challenges. Payton’s disorder — early-onset SMA — is a prime example of this type of disorder, but it’s not alone.
Metabolic and mitochondrial muscle diseases, as well as congenital muscular dystrophies, Friedreich’s ataxia and myotubular myopathy are among the other conditions in which spinal curvatures may become serious enough to require treatment when a child is still quite young.
Neuromuscular weakness causes large and early curvatures
 |
| Spinal curvatures associated with SMA can occur very early in childhood, says neurologist Tom Crawford. |
 |
| Scoliosis in neuromuscular disease is different from scoliosis without an underlying disorder, emphasizes orthopedic surgeon Paul Sponseller. |
 |
| Spinal curvatures associated with neuromuscular disorders tend to be long and C-shaped, says orthopedic surgeon Brian Snyder. |
Neurologist Tom Crawford, co-director of the MDA Clinic at Johns Hopkins University in Baltimore, where he’s an associate professor of neurology and pediatrics, has a special interest in SMA-associated scoliosis.
“When you have weakness of your long back muscles, which is one of the key features of SMA, that means that you’ve got gravity pulling on the spine, unopposed by the forces that would normally be exerted by muscles. As the curvature worsens, the rate of decline of the curvature increases. With each additional few degrees of curvature, the pull of gravity is that much stronger. So things look subtle, then mild, then not so great, and then there’s a sort of collapse of the spine.”
Unfortunately, Crawford notes, that can occur in very early childhood in this disease.
Paul Sponseller, an orthopedic surgeonand chief of Pediatric Orthopaedics at Hopkins, works closely with Crawford and receives many referrals for spinal curvature management from his clinic.
“A lot of patients unfortunately end up with spinal deformities, so we manage them with different things, including bracing and monitoring and, at times, surgery,” Sponseller says.
He notes that the scoliosis that occurs in neuromuscular disease is quite different from the kind that occurs in adolescents without underlying disorders, known as idiopathic scoliosis, meaning scoliosis arising from an unknown cause.
“With idiopathic scoliosis, only a limited portion of the spine is affected,” Sponseller says, while neuromuscular scoliosis usually affects the entire spine.
“Neuromuscular curves tend to be very long,” says Brian Snyder, an orthopedic surgeon at Boston Children’s Hospital. “They start at the base of the neck and go all the way down to the pelvis. If you think of a column of beads that are connected, if you don’t have sufficient muscle strength to help support those beads in a vertical line, they’ll tend to collapse, typically into a C shape. It’s like a beam buckling.”
In contrast, he says, idiopathic curves, which occur mostly in girls around the time of their adolescent growth spurt, are usually S-shaped and involve only part of the spine.
Bracing can buy time before surgery
For growing children with neuromuscular scoliosis, Crawford says he strongly believes in TLSOs — “thoraco-lumbar-sacral orthoses” — a type of back brace that goes from the chest to the pelvis and exerts force against the spine. In fact, it surprises him that not every expert shares his opinion, but he believes that’s because some orthopedists confuse idiopathic and neuromuscular scoliosis.
“It’s true that TLSOs do nothing for idiopathic scoliosis, which is probably driven by some asymmetric [unbalanced] growth of the spine,” he says. “If the spine is growing asymmetrically, you’re not going to fix that by pushing on the outside of the skin. It’s just going to continue to grow, and people will then find the brace uncomfortable.
“But if the driving force for the curvature is the force of gravity, and you’re successful at wearing a well-fitting TLSO whenever gravity is in force — whenever you’re upright — then it really does prevent the conversion from a slowly progressive curvature to a collapse.”
Crawford concedes that curvatures often progress while a child is wearing a TLSO, but they do so slowly. “It prevents the rapid-phase progression,” he says, buying time and allowing growth.
In boys with DMD, however, Crawford doesn’t typically recommend a brace, as DMD-related scoliosis generally becomes a problem in adolescence when “they’re at skeletal maturity or close to it, and there’s no reason to do the TLSO.” Instead, Crawford, in consultation with an orthopedic surgeon, generally recommends immediate spinal fusion surgery for teens with DMD.
Postponing spinal surgery in children with SMA and other conditions that can cause early-onset weakness of the trunk and back muscles not only helps preserve growth but also results in a safer surgery. “Kids with SMA are fairly stable over time in terms of respiratory function,” Crawford says, “so when you push the surgery off, you just get a bigger person, with a better outcome.” (In DMD, by contrast, where respiratory function often diminishes rapidly during adolescence, postponing spinal surgery can make the procedure riskier.)
Even if a growth-permitting procedure, such as the growing rods that Payton Mueller received, is chosen, a later first surgery means fewer rod-lengthening operations will be needed. “The growing rods require a second surgery, or even a third, fourth or fifth,” Crawford says. If a family refuses bracing, he says “we will negotiate things,” but he adds that spinal surgery is “not a walk in the park,” and he’d rather a child with SMA not have too many such procedures.
The exception to the “bracing first” principle for Crawford is obese children. “If you’re skinny, then a brace that fits tightly to your chest and abdomen has pretty good purchase [mechanical hold],” he says. But when there’s a lot of fat between the brace and the spine, “it basically doesn’t do anything.” Those children, he says, may have to go to surgery earlier than thinner children.
Consequences of untreated scoliosis
Orthopedic surgeons Sponseller and Snyder both agree that bracing plays an important role in postponing surgery in neuromuscular scoliosis, but they also agree that surgery is nearly always needed eventually in this type of spinal curvature.
“Bracing is an external way of supporting the spine,” Snyder says. “It’s substituting for the role of the muscles between the ribs and adjacent to the spine. But all bracing really does is buy time. Eventually, virtually all these kids will need surgical intervention.”
Otherwise, he says bluntly, “the natural history will be an untreated scoliosis that ultimately will lead to severe deformity, severe effects on the lungs, and ultimately heart failure and death. There’s no way to pretty it up.”
Crawford cites additional important reasons to correct scoliosis in SMA and other neuromuscular disorders: “Without repair of their scoliosis, kids can’t sit in a wheelchair, and they can’t find themselves a comfortable place in bed.”
He says he remembers back in the 1980s — when surgeons were more reluctant to operate on children with neuromuscular disorders than they are now — seeing severe uncorrected scoliosis in some patients. “These guys could not be comfortable,” he says. “There was no place they could go. They couldn’t lie down, they couldn’t sit.” Nowadays, at least in the United States, he says, that outcome is “pretty rare.”
Crawford says he’s sympathetic but firm when families balk at the idea of a spinal brace. “I’m aware of the fact that this is uncomfortable and an additional encumbrance on an already compromised life,” he says, noting that sometimes braces can even prevent children from accomplishing tasks they were able to do without the brace. “But the consequences of not wearing it are even worse.”
In neuromuscular conditions, a semirigid brace, with holes cut to allow ample room for respiration and digestion, is often prescribed, although sometimes hard plastic braces are used.
At age 4, Payton Mueller started wearing a brace that was a combination of hard plastic and soft material. “They cut out a big hole for his belly, and then they cut breathing holes throughout the whole thing,” Rachele recalls. “The inside was padded, and he had extra padding in a couple of places where his body stuck out more.”
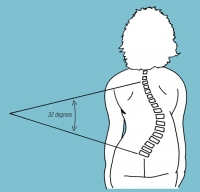 She says not wearing the brace “wasn’t an option” for Payton, who wore one until he was 9, at which point his curvature was 86 degrees and surgery was recommended. (Degrees of spinal curvature are measured as the Cobb angle, the angle at which lines drawn parallel to the top and bottom of a curvature intersect. See Cobb angle illustration, right.)
She says not wearing the brace “wasn’t an option” for Payton, who wore one until he was 9, at which point his curvature was 86 degrees and surgery was recommended. (Degrees of spinal curvature are measured as the Cobb angle, the angle at which lines drawn parallel to the top and bottom of a curvature intersect. See Cobb angle illustration, right.)
In fact, Rachele wishes they had started bracing even earlier. “This is just my thought,” she says. “But I think we could have done surgery later if we had put him in the brace earlier.”
Helping the spine to fuse
Most experts agree that the majority of children with neuromuscular scoliosis will need spinal surgery at some point, but they don’t all agree on exactly when or on what procedure is best.
“From my standpoint,” says Crawford, “If you’re staring at progressive scoliosis, the only thing worse than having a spinal fusion is not having a spinal fusion.”
The ultimate goal of spinal surgery is that the spine will fuse — the vertebrae will become firmly attached to each other — in a straightened position. But there are different approaches for accomplishing that.
The original spinal procedure employed devices known as Harrington rods, which were developed in the late 1950s by orthopedic surgeon Paul Harrington and were widely used through the 1980s.
Stainless steel rods were attached at the top and bottom of a spinal curvature and attached to the vertebrae with hooks. The rods were then tightened until the spine was straight, after which the patient was completely immobilized in a body brace or cast for months or even years until the spine fused in its new position.
“The purpose was to have the spine fuse itself,” Crawford recalls. “But it was kind of medieval.”
Next, in the 1990s, came a procedure called segmental fixation, in which vertical rods are attached at multiple points along the spine. The two rods are either dual rods, which are separate vertical rods joined together by cross-pieces; or a unit rod, which is one rod with two vertical pieces joined at the top in a U shape.
 |
| Segmental spinal fixation with dual rods, shown from the back.The surgeon used pedicle screws to secure the rods to the upper spine, a combination of screws and wires in the mid-spine, and pedicle screws for the lower spine and pelvis. |
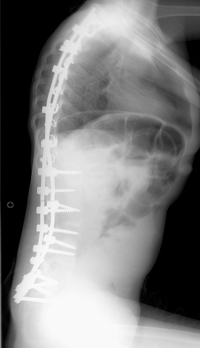 |
| Segmental spinal fixation, shown from the side. In this example, dual rods have been fixed to the spine at multiple levels with a combination of hooks, screws and wires. (X-ray photos courtesy of Brian Snyder.) |
 |
| Growing rods in a young child, shown from the front. These rods span the length of the entire spine, are secured with screws to the upper spine and pelvis, and have adjustable-length rods in between, to allow for growth. Multiple surgical procedures to lengthen the rods are necessary. |
 |
| Two VEPTR devices in a growing child, shown from the front. The VEPTRs are secured to the ribs at the upper ends and to the pelvis at the lower ends. As with growing rods, VEPTR length can be adjusted as the child grows. (X-ray photos courtesy of Brian Snyder.) |
Both unit and dual rods are made of stainless steel or titanium and inserted into the upper spine at the top and the lower spine or pelvis at the bottom, with as many anchor points in between as necessary.
Unlike the old Harrington rods, which were fixed to the vertebrae only at the top and bottom, rods used for segmental fixation can be anchored to several individual vertebrae along the spine and can apply tension to as many spinal segments as desired. They’re anchored by wires, hooks, screws or a combination of these. (See first set of X-rays, right.)
“These are put in with hooks or with pedicle screws,” Crawford explains, referring to screws that are embedded in the pedicles, the parts of each vertebra that surround the spinal cord on the left and right.
“You can put a lot of tension on each element to bring them into alignment in a way you can’t if you’re just pulling on one end and the other end,” Crawford says.
Once the rods are tightened, a bone graft — sterilized, ground bone — is sprinkled on the spine to hasten fusion.
Long periods of complete immobilization in a cast or brace are no longer required. “Now we don’t have to do that,” says Brian Snyder. “With multiple points of fixation, you don’t need to be in any sort of special brace afterward. I get my kids up immediately. They’re up in a chair the next day.”
This type of spinal fusion, like the old Harrington rod procedure, requires only one operation, with one anesthesia and one recovery period. However, it stops the growth of the spine.
“If you have to operate on a child before the age of 11 or 12, it’s not ideal,” says Sponseller. “And if you do it before the age of 10, you almost always would consider growing rods, so that you don’t stunt their growth too much.”
Jared Watson of Delmar, Del., now 12, had a spinal fusion at age 10 for SMA-related scoliosis, after wearing a brace from age 7. He hadn’t yet reached his full adult height, but his curve was 64 degrees and something had to be done. His surgeon, Paul Sponseller, wasn’t sure whether a growth-conserving surgery at this borderline age was worthwhile. He told the Watsons he would decide during the surgery which procedure was best.
“He said he would look to see,” Karen recalls. “If he felt it would benefit Jared to go back in [surgically] every year, he would put in those rods that would allow him to grow. If he felt like Jared had grown as much as he could grow, he would just do the permanent rods.”
After going through the ordeal of the surgery, she says, both she and Jared are glad the doctor opted for the fusion procedure. “After going through the whole thing, we were grateful,” Karen says. “It was hard to see him in that position, being in so much pain.” Jared spent 10 days in the hospital, and then it was another two weeks before he resumed his usual activities. His height — following the spinal straightening — is 5 feet.
Segmental fixation and fusion doesn’t “solve the growth problem,” says Crawford, but the postoperative recovery period is a lot better than it was with the old Harrington rods.
And if a child is nearly full grown, there are advantages to doing one operation instead of several.
Growth-conserving procedures
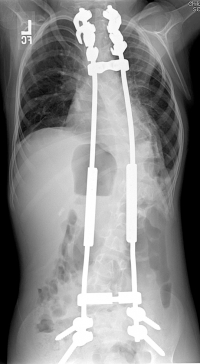
The first decade of the 21st century brought the next set of advances in scoliosis surgery: two growth-conserving procedures, one simply known as “growing rods,” and the other by its trademarked name, VEPTR, which is short for “vertical expandable prosthetic titanium rib.”
Growing rods resemble Harrington rods in that they’re attached to the spine at the top and bottom of the curve. But there the similarity ends. Growing rods are adjustable in length, although they’re set in a fixed position with each surgical procedure. (See second set of X-rays, right.)
The VEPTR attaches to the pelvis or spine on the bottom and to two or three ribs at the top. It too can be lengthened, via multiple operations, as a child grows.
“I generally like the growing rods,” says Sponseller, “because I think they’re more effective and are more likely to result in a final fusion so you don’t have to go back in and operate to fuse the patient.”
However, Snyder says, “What we think may be better with the VEPTR, is that, because you’re grabbing onto the rib, you prevent the ribs from collapsing. What happens in these weak muscle conditions is that the ribs tend to droop, and that further limits the space available for the lungs to grow.”
Different medical centers tend to specialize in one or the other technique. For now, it’s not clear which procedure is better, and Crawford believes the most important thing for families to do is find a medical center with a well-established scoliosis surgery program, whichever device or procedure they use. (See illustration.)
“There are some patients for whom the VEPTR or growing rod system may prove to be better,” Crawford says, “though for most, the difference between the two is not likely to be great. Rather than arguing about which is better, we should be determining which conditions are advantageous for one versus the other.” (Brian Snyder at Boston Children’s is involved in research to determine that.)
Payton Mueller, who underwent his initial growing-rod surgery long before his growth was complete, has had three rod-lengthening procedures so far. His second lengthening was in June 2011, but in July, the rods broke while Payton was engaged in vigorous activities and had to be replaced.
Sponseller notes that, in general, they discourage children with growing rods from engaging in contact sports, tumbling or gymnastics, which can loosen the upper and lower anchoring points, but that it’s possible for growing rods to break even with daily activities. Payton’s rods apparently broke while he was performing in a talent show, although it isn’t clear what maneuvers caused the incident.
After Payton’s third lengthening, in August 2012, spinal fluid started leaking from his surgical incision, and it was discovered that he had a tear in the outer covering of the spinal cord. “They had to reopen Payton’s incision and do some exploring,” Rachele says. “It was hard to find where the tear was, but they found it, patched it and sewed it up. He was in the hospital for another week after that, and then he was fine.”
Despite the complications, both Rachele and Payton are happy with their choice of growing rods over fusion. Because his trunk and limbs are all still growing at the same rate, his body parts have stayed in proportion to each other, she notes.
“It seems to me, from the parents that I’ve talked to, that the kids that were not fused but had the growing rods are healthier,” she says. “I don’t know if that’s true or not, but it seems as if they are. Their organs are where they’re supposed to be. Those [organs] are still growing. They don’t stop growing just because you fuse the spine.”
Payton says the initial rod insertion surgery was much more painful than the subsequent rod lengthenings and that he would recommend the growing rods. “As soon as you’ve done it once or twice, it’s OK, because you get used to it,” he says. Compared to how he felt before the rods, he says, “I can sit up straighter. I just feel better. I can breathe easier, and my neck doesn’t hurt as bad anymore.”
Fusion may be necessary at full height
What to do about a VEPTR or growing rod “graduate” — someone who has had a growth-conserving procedure and has now reached his or her full height — is a question that remains open for debate, says Brian Snyder. Whether or not a final procedure to fuse the spine is necessary is, for now, decided on an individual basis, taking into account factors such as the child’s activity level.
“There are three different ways you can go,” Snyder says. “You can either convert to a regular spine fusion; you can leave the rods in and not do anything more; or you can expose the spine, lay in bone grafts, and just use the rods to keep things straight while the bone heals.” Snyder adds that there are ongoing studies to determine which approach is best under which circumstances.
For a child who’s full grown and not putting much demand on his growing rods or VEPTR, “sometimes we can just stop,” Snyder says. “The metal devices are strong enough to support the trunk, and you don’t have to do anything more.”
A “low-demand” patient, Snyder says, would be a child who’s “at most getting up into a stander an hour or two a day and otherwise not doing anything that puts them at any significant risk for breaking their hardware.”
In a child who’s moderately active, it may suffice to keep the existing hardware in place and sprinkle some pulverized bone over the spine to facilitate self-fusion of the vertebrae. Snyder defines “moderately active” as a child who walks, with or without an assistive device, and participates in adaptive physical education and physical therapy.
In a child who’s very active, it may be necessary to do a full spinal fusion. Snyder defines “very active” as a child who walks and runs with minimal or no assistive devices and participates in sports.
The risks of surgery
Spinal surgery, while safer and less arduous than it used to be, is still risky and painful, says Tom Crawford.
“It’s a big surgery,” he says of procedures to insert new hardware. (Although adjustments to lengthen existing hardware are not as complex, they still require anesthesia and pose risks.)
“The potential is there for increased need for respiratory support” [in the postoperative period], Crawford says, usually in the form of noninvasive, positive-pressure ventilation, such as BiPAP. But at times, invasive ventilation via a tracheostomy tube (inserted through the skin into the windpipe) may be necessary.
 “Sometimes if the lungs aren’t vigorously re-expanded, the patient will need a trach,” says Sponseller. “It can be permanent, or it may be removed in a couple of years.”
“Sometimes if the lungs aren’t vigorously re-expanded, the patient will need a trach,” says Sponseller. “It can be permanent, or it may be removed in a couple of years.”
Snyder concurs. “These patients often don’t have healthy lungs to begin with,” he says. “If you don’t have a healthy lung to begin with, and you’ve had lots of hospitalizations for pneumonia, you’re going to have the same complications in the immediate postoperative period.”
He adds, “Before I even do the surgery in these kids, I meet with my pulmonologist and decide how their respiratory function is. If the respiratory function is so diminished that we think there’s a high likelihood that they may not come off the ventilator [used during surgery], we’ll do a tracheostomy up front.”
During surgery, the main complication is bleeding, which may require blood transfusions. “Blood is fairly safe — we know how to screen for HIV and hepatitis — and I have no problem giving it to my patients,” Snyder says. Still, the surgery requires caution and meticulous attention to changes in blood pressure, especially if there are cardiac aspects to a child’s disease.
Another potential surgical complication involves the instrumentation — “If I put in a pedicle screw in the wrong place, I can cause a neurologic injury,” says Snyder. He says the incidence of permanent injury to the spinal cord during scoliosis surgery is “probably less than 1 percent,” but “it can happen.”
During the surgery, Snyder’s team, like those at other major medical centers, monitors spinal cord function. “We do something called somatosensory evoked potentials,” he says, to measure the sensory function of the spinal cord. (Evoked potentials are electrical signals generated by the nervous system in response to stimulation.)
“In kids who have enough motor function, we also do motor evoked potentials,” he notes. “We get lots of X-rays, and we monitor the spinal cord during the surgery to make certain that as we’re putting in the hardware and straightening the spine we’re not doing anything to injure the spinal cord.”
Snyder says that VEPTR procedures cause less direct pulling on the spinal cord than spinal rods do but more pulling on the nerves controlling arm movement and sensation, with associated risk of damage to those nerves.
Anesthesia is another potential risk. Snyder notes, “Your anesthesiologist has to be experienced. You need to avoid halothane [a type of anesthetic gas] in some of the myopathies, and you need your anesthesia team to be well-skilled.”
In children with cardiac abnormalities, he says, “we’ll do central venous lines where we can measure their central venous blood pressure, and we’ll use esophageal echocardiography [imaging of the heart through the esophagus] to measure their ventricular [pumping chamber] function.”
After the procedure, Snyder says, “wound infection can be a devastating complication that interferes with the success of the surgery. If that happens, you have to open up the spine, wash it out multiple times, and sometimes even take out the hardware to try to clear the infection.”
Other types of infection — for instance, of the lung and urinary tract — also can occur, and they can even spread to the site of the surgery.
 Postoperative pain has to be managed carefully, by doctors who understand the child’s neuromuscular disorder and the adverse effects some pain medications can have on breathing.
Postoperative pain has to be managed carefully, by doctors who understand the child’s neuromuscular disorder and the adverse effects some pain medications can have on breathing.
“There are a lot of places that problems can happen,” Snyder says. “Most of the complications are not associated with the initial surgery itself but with postop medical problems that sneak up that need to be anticipated and addressed up front.
“I think this kind of surgery in this population of children should only be performed at a big institution that has an intensive care unit and staff that are used to taking care of children with neuromuscular disorders and lots of comorbidities [coexisting conditions]. It should only be done at a place where you have neurologists, cardiologists, pulmonologists and intensivists [intensive care specialists], and the surgery should be performed by somebody who’s done it a lot.”
Postop adjustments may take time
In addition to the strictly medical complications, families need to be briefed that there may be some loss of comfort and even loss of function after surgery to correct neuromuscular scoliosis, Crawford says.
 For one thing, he notes, children may have been able to do things with a curved spine that they can’t do with a straight one.
For one thing, he notes, children may have been able to do things with a curved spine that they can’t do with a straight one.
“You can’t do all those little wiggle things,” he says. “When you sit, you wiggle your tush around and do all kinds of things to feel more comfortable. And now they can’t. A lot of what you used to do to accommodate to being weak may be taken away by the fusion. The first month or so after surgery, getting used to the new body, is a pretty rugged time — tough on kids and on their parents.”
Also, he concedes, there can be permanent loss of muscle function from prolonged immobility associated with the surgery, even though recovery times are shorter than they used to be. “A lot of kids will lose something in the postoperative period and then recover only half of it,” he cautions.
That may be what happened to Jared Watson, who says, “Before, I could use my arms a lot more, even with the brace. Afterward, my arms were terrible. The rod in there straightened me out a lot, but my arms got weaker from the recovery.”
Crawford also warns parents of what the surgery and recovery period will mean for them. “There’s a lot of work involved in mobilizing people,” he says. “Every parent is going to have to deal with the fact that they’re going to have to take time off.”
No fun, but worth doing
Scoliosis surgery is “not fun,” Crawford says. “And the specifics of how we go about doing it aren’t settled yet. There’s plenty for smart people to work on to get the right answers.”
But from his point of view, most children with neuromuscular scoliosis are far better off with it than without it, and the more growing time a child has prior to surgery, the better the outcome generally is.
Despite losing some arm strength, Jared Watson says he’d advise children in situations like his to have scoliosis surgery.
“The main thing is not wearing the brace,” he says. “You get straighter. You can sit up straighter. There are a lot of things you can do. It’s pretty good. It’s been great for me.”
Two Fusions May Allow Additional Spinal Growth
A strategy that doesn't apply to too many children with neuromuscular scoliosis — but may fit the bill for some — is to have two separate operations to fuse different parts of the spine.
 That was the approach taken by the surgeon for Katelyn Cross of Malone, Fla. Katelyn, who has Friedreich’s ataxia, developed two spinal curvatures — an upper and a lower one — around age 9. As the curves progressed, she was frequently troubled with digestive and respiratory difficulties.
That was the approach taken by the surgeon for Katelyn Cross of Malone, Fla. Katelyn, who has Friedreich’s ataxia, developed two spinal curvatures — an upper and a lower one — around age 9. As the curves progressed, she was frequently troubled with digestive and respiratory difficulties.
After four years of bracing, Katelyn had two surgeries, two years apart. The first, when she was 13, fused her upper spine, which had an 80-degree curvature. The second, at age 15, fused her lower spine, which had about a 50-degree curve at the time of the first surgery and had progressed to 63 degrees two years later. Separating the fusions by two years allowed the lower spine to continue growing after the severe upper curvature was repaired. A downside, however, is that two fusion operations were required.
Now 17, Katelyn is 5 feet 3 inches tall and still has “a little curve,” says her mother, Angela. “They couldn’t get all of it out, but she doesn’t have difficulty with acid reflux anymore, and her breathing’s OK.”
“Of course the surgeries were scary,” Angela says. “But after she healed up, she knew they were the best thing in the long run.” Besides improving her health and well-being, Katelyn now can wear clothes that didn’t fit her right before the surgery because of the curve. “It’s been a positive experience,” Angela says.
Bracing Alone May Suffice for Small Curves
Very occasionally in a child with neuromuscular scoliosis, a brace will suffice, and surgery can be avoided altogether.
 For Christine Westendorf of West Dundee, Ill., now a 28-year-old public relations professional, that was the case.
For Christine Westendorf of West Dundee, Ill., now a 28-year-old public relations professional, that was the case.
Westendorf has both type 2 myotonic dystrophy and myotonia congenita — an unusual combination of disorders, neither of which usually causes profound weakening of the spine-supporting musculature. Neither diagnosis was made until adulthood, but a relatively small spinal curvature (25 degrees) was identified during an annual physical exam when she was 10 years old.
She wore a series of back braces that had to be changed as she grew until she was 13, at which point her treatment stopped.
“They decided bracing would be the best option to keep the curvature from becoming worse than it was,” Westendorf says. “I was going through the adolescent growth spurt at that time. My left shoulder severely drooped more than my right shoulder, and the brace had a thing built in on the side for my left arm, so my left arm would rest on that.”
Nowadays, she says, her back isn’t completely straight, but she has no major problems. Wearing the brace, she says, was “tough,” but she’s glad she did it.
Got Questions About Spinal Surgery for Children and Teens?
Watch the MDA Webinar “Straightening the Growing Spine,” held Jan. 22, 2013, and featuring pediatric neurologist Tom Crawford, orthopedic surgeon Paul Sponseller, and parent Rachele Krebsbach (all interviewed in this article).
MDA Resource Center: We’re Here For You
Our trained specialists are here to provide one-on-one support for every part of your journey. Send a message below or call us at 1-833-ASK-MDA1 (1-833-275-6321). If you live outside the U.S., we may be able to connect you to muscular dystrophy groups in your area, but MDA programs are only available in the U.S.
Request Information